Eight 2023 acetyl-L-carnitine / L-carnitine papers, starting with three healthy human studies:
“Thirty healthy volunteers aged between 19 and 52 years were divided randomly into two equal groups, one of which received 1000 mg of L-carnitine (LC) per day over a 12-week period. Total cholesterol and HDL-C increased significantly after supplementation. LC could be useful in impeding development of heart diseases in subjects with low HDL-C.”
https://journaljammr.com/index.php/JAMMR/article/view/5166 “L-Carnitine Increases High Density Lipoprotein-Cholesterol in Healthy Individuals: A Randomized Trial”
Rationale for dose selection wasn’t provided, and the possibility of limited results due to poor study design wasn’t mentioned.
“This study examined effects of 12 weeks of LC supplementation on bone mineral density (BMD) and selected blood markers involved in bone metabolism of postmenopausal women participating in a resistance training (RT) program. Participants’ diets were supplemented with either 1 g of LC-L-tartrate and 3 g of leucine per day (LC group) or 4 g of leucine per day as a placebo (PLA group), in a double-blind fashion.
Because the study protocol consisted of both exercise and supplementation, some favorable changes in the BMD could be expected. However, it was not possible to detect them in the short study period. No significant modification in BMDs of the spine, hip, and total skeleton and no differences between groups in one-repetition maximum could be due to the relatively short duration of the RT intervention.”
https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-023-00752-1 “Effect of a 3-month L-carnitine supplementation and resistance training program on circulating markers and bone mineral density in postmenopausal women: a randomized controlled trial”
Same comments as the first study regarding no rationale for dose selection, and no mention that limited results were possibly due to an inadequate dose.
In a letter to the editor, a researcher took issue with a study’s methodology:
“Based on finding that intravenous provision with carnitine alone does not increase muscle carnitine accretion, and on the above-reevaluated data, it appears that the basis for carnitine with caffeine being able to increase muscle carnitine levels, and thereby manipulation of muscle metabolism and exercise performance, is uncertain.
Carnitine bioavailability in any group would have been 9.5%. This assessment would be in line with previously recorded values of 5%–18% carnitine bioavailability. It is firmly believed that low carnitine bioavailability is attributable to the inability of kidneys to reabsorb carnitine when the threshold concentration for tubular reabsorption (about 40–60 μmol/L) has passed this value.
The authors’ proposed long-term use of carnitine supplementation as an aid to improve fat oxidation in type II diabetes also seems to lack provision.”
https://physoc.onlinelibrary.wiley.com/doi/10.14814/phy2.15736 “LTE: Does caffeine truly raise muscle carnitine in humans?”
Two genetic studies:
“Our findings suggest that humans have lost a gene involved in carnitine biosynthesis. Hydroxytrimethyllysine aldolase (the second enzyme of carnitine biosynthesis) activity of serine hydroxymethyl transferase partially compensates for its function.”
https://www.researchsquare.com/article/rs-3295520/v1 “One substrate-many enzymes virtual screening uncovers missing genes of carnitine biosynthesis in human and mouse”
“Reported prevalence of primary carnitine deficiency (PCD) in the Faroe Islands of 1:300 is the highest in the world. The Faroese PCD patient cohort has been closely monitored and we now report results from a 10-year follow-up study of 139 PCD patients.
PCD is an autosomal recessive disorder that affects the function of organic cation transporter 2 (OCTN2) high-affinity carnitine transporters, that localizes to the cell membrane and transport carnitine actively inside the cell. Without proper functioning OCTN2 carnitine transporters, renal reabsorption of carnitine is impaired, and as a consequence, patients suffering from PCD have low plasma levels of carnitine. This can disturb cellular energy production and cause fatigue, but also in extreme cases lead to cellular dysfunction and severe symptoms of coma and sudden death.
PCD patients seem to adhere well to L-carnitine treatment, even though they have to ingest L-carnitine tablets at least three times a day. Overall mean L-carnitine dosage was 66.3 mg/kg/day.”
https://onlinelibrary.wiley.com/doi/10.1002/jmd2.12383 “Patients with primary carnitine deficiency treated with L-carnitine are alive and doing well—A 10-year follow-up in the Faroe Islands”
The average daily dose is (66.3 mg x 70 kg) = 4,641 mg. A third of this dose would be about 1.5 g.
The first study of Acetyl-L-carnitine dosing also suggested dosing L-carnitine three times a day because of 10-20% bioavailability.
A study with unhealthy humans:
“This retrospective study analyzed medical records of adult patients between March 2007 and April 2019, with presenting complaints of fatigue and lethargy. Acetyl-L-carnitine has physiological functions similar to L-carnitine but has higher bioavailability and antioxidant properties. This study confirmed that a triple combination therapy with γ-linolenic acid, V. vinifera extract, and acetyl-L-carnitine can improve arterial stiffness in patients.
Our study had some limitations:
- The study population may not be representative of the entire Korean adult population.
- The study did not have a medication-free control group. Instead, the comparison group comprised patients with medication compliance <80%.
- Drop-out rate of the triple-combination therapy (46.2%, 147/318) was relatively high, indicating the possibility of bias due to loss to follow-up.
- The study did not consider lifestyle factors such as smoking, diet, and physical activity level, which may affect arterial stiffness.
- The study did not examine interactions among drugs comprising the combination therapy, although all drugs are known to positively impact blood vessels.”
https://onlinelibrary.wiley.com/doi/10.1111/jch.14708 “Efficacy of γ-linolenic acid, Vitis vinifera extract, and acetyl-L-carnitine combination therapy for improving arterial stiffness in Korean adults: Real-world evidence”
This study’s acetyl-L-carnitine dose was 500 mg three times a day.
Wrapping up with two rodent studies:
“Acetyl L-carnitine (ALCAR) has proved useful in treatment of different types of chronic pain with excellent tolerability. The present work aimed at evaluating the anti-hyperalgesic efficacy of ALCAR in a model of persistent visceral pain associated with colitis.
The acetyl group in the ALCAR molecule can enhance cholinergic signalling by promoting synthesis of neurotransmitter acetylcholine, which plays an important role in both the enteric and central nervous systems. Acetylcholine signalling has significant antinociceptive effects in development of visceral pain, so it has been proposed as a therapeutic target.

ALCAR significantly reduced establishment of visceral hyperalgesia in DNBS-treated animals, though the interventive protocol showed a greater efficacy than the preventive one.
- The interventive protocol partially reduced colon damage in rats, counteracting enteric glia and spinal astrocyte activation resulting from colitis.
- The preventive protocol effectively protected enteric neurons from inflammatory insult.
These findings suggest the putative usefulness of ALCAR as a food supplement for patients suffering from inflammatory bowel diseases.”
https://www.mdpi.com/1422-0067/24/19/14841 “Anti-Hyperalgesic Efficacy of Acetyl L-Carnitine (ALCAR) Against Visceral Pain Induced by Colitis: Involvement of Glia in the Enteric and Central Nervous System
This study cited multiple animal studies that found acetyl-L-carnitine was effective for different types of pain. I’ve taken it every day for nineteen years, and haven’t noticed that effect.
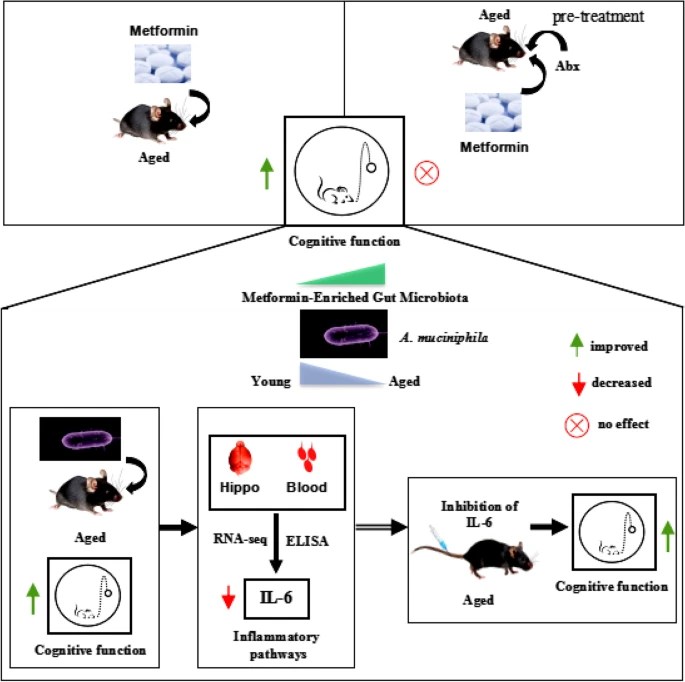
“Repetitive mild traumatic brain injuries (rmTBI) may contribute to development of neurodegenerative diseases through secondary injury pathways. Acetyl-L-carnitine (ALC) shows neuroprotection through anti-inflammatory effects, and via regulation of neuronal synaptic plasticity by counteracting post-trauma excitotoxicity. This study aimed to investigate mechanisms implicated in etiology of neurodegeneration in rmTBI mice treated with ALC.
ALC is an endogenously produced carnitine metabolite present in tissue and plasma, and readily crosses the blood brain barrier, unlike its unacetylated form. ALC is also a commonly available nutritional supplement, with a known safety profile, and had been well-studied for its role in aiding β-oxidation of long chain fatty acids in the mitochondria.
While some studies have shown promise for improving clinical and psychometric outcomes in individuals with probable Alzheimer’s disease (AD) and mild cognitive impairment, other studies that included participants with moderate AD progression were less conclusive. It may be that this lack of improvement is related to a therapeutic window of opportunity. Once neurodegenerative mechanisms have commenced, a reversal of these processes is not attainable.
There is currently a lack of evidence for safe therapeutics that can be administered long-term to reduce the risk of individuals developing cognitive and neuropsychological deficits after rmTBIs. Prophylactic ALC treatment in a paradigm of neurotrauma may be a way to maximize its therapeutic potential.
While brain structures display differential vulnerability to insult as evidenced by location specific postimpact disruption of key genes, this study shows correlative mRNA neurodegeneration and functional impairment that was ameliorated by ALC treatment in several key genes. ALC may mitigate damage inflicted in various secondary neurodegenerative cascades – confirmed by improvements in behavioral and cognitive function – and contribute to functional protection following rmTBI.”
https://www.frontiersin.org/articles/10.3389/fphar.2023.1254382/full “Repetitive mild traumatic brain injury-induced neurodegeneration and inflammation is attenuated by acetyl-L-carnitine in a preclinical model”
I read many traumatic brain injury papers earlier this year, but only curated two in Brain endothelial cells. I came away thinking that there’s no permanent recovery from TBIs, as just symptoms are effectively treated.
Most TBIs happen to old people who have diminished brain reserves. I didn’t see studies that factored in evidence of what happened earlier in injured people’s lives that created TBI susceptibility but wasn’t remembered.
Unlike other years, I haven’t watched any football this season. It’s unsettling that transient entertainment value continues to take precedence over permanent effects on players’ lives.