Continuing Plasmalogens Week with three 2025 papers, starting with a rodent study of genetically deleting a plasmalogen catabolizing enzyme:
“In this study, we investigated the impact of global and tissue-specific loss-of-function of a plasmalogen catabolizing enzyme, lysoplasmalogenase (TMEM86B), on circulatory and tissue lipidomes. Mice with homozygous global inactivation of Tmem86b (Tmem86b KO mice) were viable and did not display any marked phenotypic abnormalities.
Tmem86b KO mice demonstrated significantly elevated levels of plasmalogens alkenyl phosphatidylethanolamine (PE(P)) and alkenyl phosphatidylcholine (PC(P)), as well as lysoplasmalogens, in the plasma, liver, and natural killer cells compared to their wild-type counterparts. The endogenous alkenyl chain composition of plasmalogens remained unaltered in Tmem86b KO mice. Consistent with the global knockout findings, hepatocyte-specific Tmem86b knockout mice also exhibited increased plasmalogen levels in the plasma and liver compared to their floxed control counterparts.
Plasmalogens may be synthesized locally within various tissues, with each organ possessing the necessary enzymatic machinery to regulate its own plasmalogen levels. Plasmalogens are important structural constituents of the biological membranes of animals and certain anaerobic bacteria, and have several well-described functions, including regulating membrane dynamics and vesicular cholesterol transport and homeostasis.
- One of the most interesting features of plasmalogens is their endogenous antioxidant activity, which is mostly due to the vinyl ether bond, which can scavenge reactive oxygen species and thereby protect other biomolecules from oxidative damage.
- They increase the gene expression of multiple antioxidant enzymes to protect against chemically induced cytotoxicity and lipid peroxidation in cultured hepatocytes.
- Plasmalogen derivatives such as polyunsaturated fatty acids (AA or DHA) and lysoplasmalogens can act as lipid mediators for multiple cellular signaling activities.
- Plasmalogens are important for phagocytosis of macrophages, lipid droplet formation, and development and function of neuromuscular junctions.
- They play vital roles in mediating immune responses, and mitochondrial fission to regulate adipose tissue thermogenesis, and protecting neuronal cells against cell death and inflammation.
All of these are suggestive of a critical role played by plasmalogens in maintaining cellular homeostasis.
While plasmalogen anabolism is well defined, its catabolism has been less studied. During catabolism, plasmalogens are deacylated by the action of a calcium-independent phospholipase A2 enzyme (iPLA2) to produce lysoplasmalogens. However, cytochrome C has also been shown to act as a plasmalogenase under certain circumstances.
The amount of lysoplasmalogens in cells is tightly regulated either by reacylation into plasmalogens through a coenzyme A-independent transacylase, or by degradation into fatty aldehydes and glycerophospholipids by an alkenyl ether hydrolase commonly known as lysoplasmalogenase. Lysoplasmalogenase is a microsomal transmembrane enzyme highly specific for lysoplasmalogens, and has no activity against plasmalogens.

While research on the distinct biological functions of lysoplasmalogens and plasmalogens is lacking, some reports indicate potential toxic effects of lysoplasmalogens. Degradation products of lysoplasmalogens, such as fatty aldehydes, are highly reactive electrophilic compounds that can form toxic adducts with cellular proteins and lipids. These interactions can lead to cellular dysfunction and contribute to various pathological conditions. Their accumulation in ischemic/reperfused tissues has been associated with cellular damage.
However, we observed that the amount of lysoplasmalogens as a proportion of total plasmalogens in the liver of Tmem86b KO mice was only ∼3.5%, indicating that elevated lysoplasmalogens are rapidly converted into plasmalogens within the liver. In adipose tissue-specific Tmem86a KO mice, which also exhibited higher lysoplasmalogens, no toxic effects were observed. Instead, these mice showed elevated mitochondrial oxidative metabolism and energy expenditure, offering protection from high-fat diet-induced metabolic dysfunction. These findings suggest that any potential toxic effects of lysoplasmalogens are largely mitigated by their rapid reacylation into plasmalogens.
This study enhances our understanding of regulatory mechanisms governing plasmalogen metabolism, and highlights the potential of targeting Tmem86b to therapeutically raise plasmalogen levels.”
https://www.jlr.org/article/S0022-2275(25)00068-9/fulltext “Modulation of endogenous plasmalogens by genetic ablation of lysoplasmalogenase (Tmem86b) in mice”
An independent researcher published a commentary on the above study:
“While the biosynthesis of this particular lipid subclass, starting in the peroxisomes and ending at the endoplasmic reticulum, has been the subject of extensive research, the degradation pathway of these compounds remains to be further elucidated. Plasmalogen breakdown is a complex process involving enzymatic hydrolysis, oxidative cleavage, and possibly also a recycling mechanism.
A fundamental unresolved question in the field of plasmalogen catabolism is which of the two possible reaction routes is actually the more important one. Either 1) directly via plasmalogenase or 2) via a deacylation step by a plasmalogen-specific phospholipase A2 (cPLA2, PLA2G4A), yielding a lysoplasmalogen as the first degradation product, and subsequent hydrolysis of the ether bond by a lysoplasmalogenase such as TMEM86A and TMEM86B. It is also unclear how these pathways interact or compensate for each other, how they are regulated, and whether they are tissue- or cell type–specific.
To make the story even more complex, a CoA-independent transacylase activity was described that reacylates lysoplasmalogen intermediates back to plasmalogens by transferring polyunsaturated fatty acids to the vacant sn-2 position of ether lysophospholipids. But no gene for this enzyme has so far been identified.

Why is plasmalogen breakdown so important? Disturbances in plasmalogen metabolism are associated with several human disorders. Neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis have been shown to be associated with reduced levels of plasmalogens.
Unfortunately, it is still too early to draw conclusions about the individual roles of TMEM86A and TMEM86B, as their cellular localisation and function are not sufficiently studied, and reliable antibodies for these proteins are not yet available. Localization of the two TMEM86 homologs overlaps to some extent, as shown, for example, by their gene expression in small intestine. However, whether one isoform is able to compensate for a deficiency in the other is uncertain, and was not found in small intestine of Tmem86b knockout mice [in the above study].
In contrast to the two proteins TMEM86A and TMEM86B, cytochrome c is much better studied. It is associated with the inner mitochondrial membrane, and can be released into the cytosol during apoptosis. It has a wide tissue distribution with most abundant gene expression levels in the digestive tract and heart.“
https://www.jlr.org/article/S0022-2275(25)00074-4/fulltext “Plasmalogen. Quo vadis?”
The statement “no gene for this enzyme has so far been identified” revealed a paradigm. But maybe what’s being observed evolved before genes?
One example of this principle is from the 1966 https://www.science.org/doi/10.1126/science.152.3720.363 “Evolution of the Structure of Ferredoxin Based on Living Relics of Primitive Amino Acid Sequences” which provided evidence pointing to heme protein evolution beginning before gene evolution. Its abstract included this statement:
“We explain the persistence of living relics of this primordial structure by invoking a conservative principle in evolutionary biochemistry: The processes of natural selection severely inhibit any change in a well-adapted system on which several other essential components depend.”
Maybe the process of reassembling plasmalogen breakdown products back into plasmalogens without involving a specific gene likewise became essential?
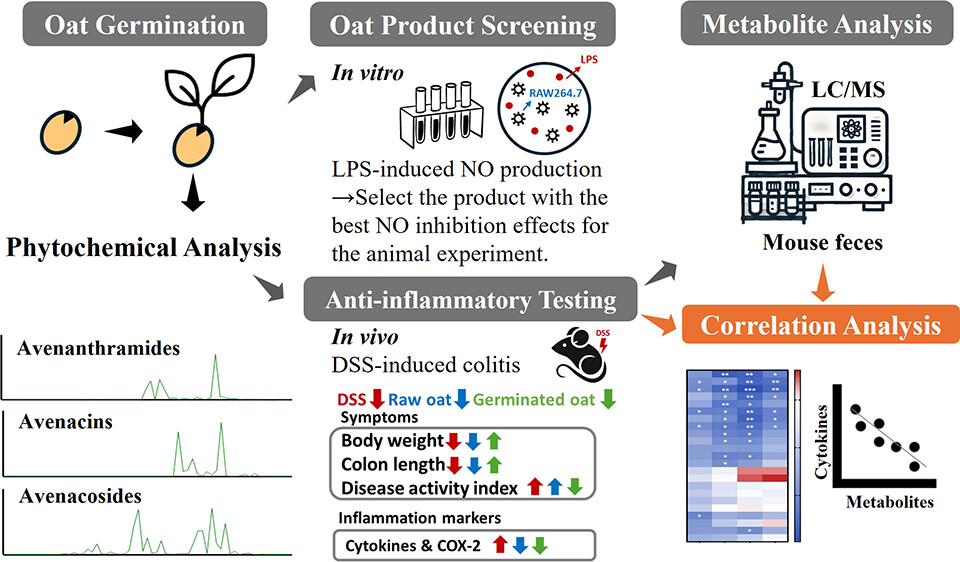
A role of plasmalogens in diabetic kidney disease was found in a third study that investigated a genetic rodent model of diabetes:
“Diabetic nephropathy (DN) represents a frequent cardiovascular complication of diabetes, affecting about 20–50% of individuals with the disease. Globally, it constitutes a primary etiology for end-stage kidney disease (ESKD) and chronic kidney disease (CKD), while also serving as a significant independent risk factor for cardiovascular morbidity and mortality.
Although intensive management strategies targeting blood pressure and glucose levels demonstrably attenuate the risk of DN development, they do not confer complete protection. This residual risk strongly implicates pathogenic factors beyond impaired glucose metabolism and hemodynamic alterations in DN pathogenesis.
In the present study, we employed the db/db mice as the DN model. When compared to other diabetes models, such as those induced by streptozotocin (STZ) or high-fat diet combined with STZ, the db/db model more accurately recapitulates the pathological features of human type 2 diabetes mellitus (T2DM). It also possesses a stable genetic background, making it particularly well-suited for the investigation of diabetes complications.
Transcriptomics revealed extensive dysregulation of metabolic and lipid regulatory pathways in db/db. Lipidomics uncovered pronounced abnormalities in cardiolipin species composition and plasmalogen profiles. Transcriptome-lipidome integration demonstrated impaired phosphatidylcholine (PC) biosynthesis, mechanistically linked to dysregulation of choline phosphotransferase 1 (chpt1), which correlated significantly with compromised tissue regeneration capacity.

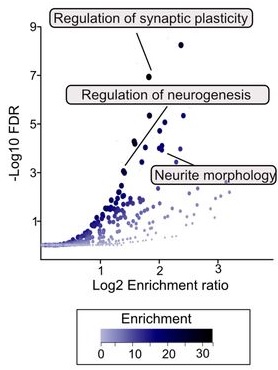
Volcano plot analysis delineated specific lipid alterations, particularly in plasmalogen species in plasmalogen lipids. Plasmenylcholines (plas-PC) and plasmenylethanolamine (plas-PE) containing n-3 polyunsaturated fatty acids (PUFAs) were significantly decreased in the kidneys of db/db mice. Conversely, plas-PCs and plas-PEs esterified with n-6 PUFAs showed substantial accumulation in diabetic kidneys.
In conclusion, the highly sensitive and extensively targeted UHPLC-MS/MS methodology enabled a more in-depth characterization of renal metabolic and lipid perturbations in db/db mice. These alterations principally reflect the sustained inflammatory milieu and compromised antioxidant defenses characteristic of DN renal tissues.”
https://www.csbj.org/article/S2001-0370(25)00301-0/fulltext “Multi-omics characterization of diabetic nephropathy in the db/db mouse model of type 2 diabetes”